Mention the word “aging” to most people and it conjures up thoughts of aches, pains, diseases, and a reduced quality of life.
Though many older adults live happy and fulfilling lives, medical illness and associated disability become more common with increasing age. But as the thousands of elderly patients from Connecticut and neighboring states who have entrusted their physical and mental well-being to geriatricians at the UConn Center on Aging have learned, the negatives that come with aging can be well managed with the right medical care, allowing people to find more enjoyment and fulfillment in their senior years.
Geriatric medicine, which began in the United Kingdom, emerged as a field in this country in the 1980s, around the time that the UConn Center on Aging was established, making it one of the first and largest multidisciplinary centers of its kind in the country.
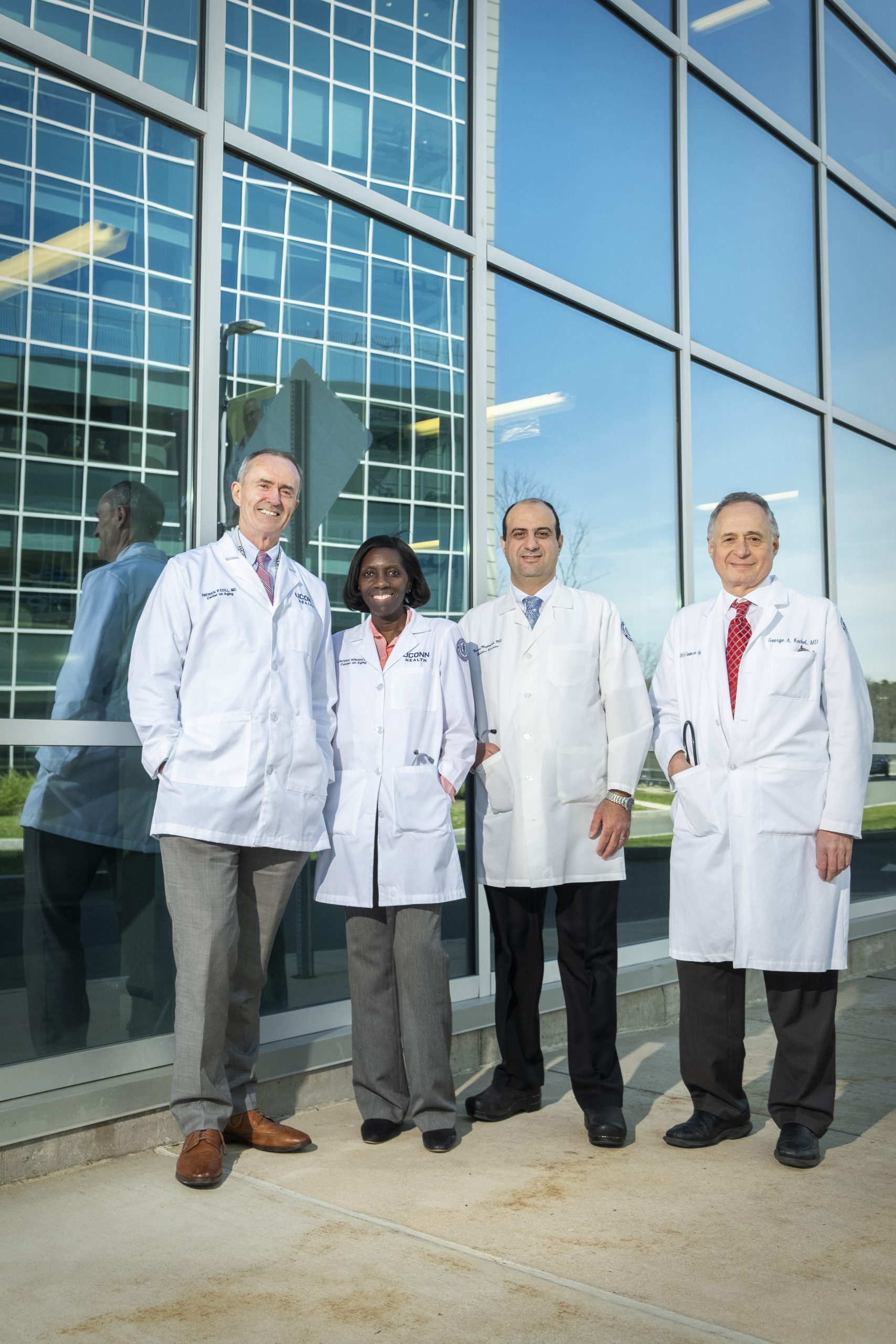
Focusing on treating patients with kindness and compassion, listening to their concerns and involving them in their own care, the center’s team of board-certified geriatricians provides comprehensive, individualized care for aging adults. These physicians “consider the full picture of each patient’s medical, social, family, and psychological needs and help coordinate the services that are needed to lead a healthy, fulfilling life,” notes the center’s website.
The center also operates a nationally recognized, interdisciplinary research program aimed at minimizing or preventing disability in older adults and finding better ways to preserve patients’ physical and cognitive function.
George A. Kuchel, M.D., FRCP, AGSF, director of the center, points out that people “don’t all age the same way.” So while the bulk of the center’s patients are well over age 65 – six of every eight patients are over age 85, many are in their 90s, and still others have passed 100 – there are younger adults with medical and psychological needs who also qualify for this care.
Patrick Coll, M.D., a geriatric specialist at the center, says “the signature syndrome for our specialty, which we term multiple co-morbidity, involves four or more medical conditions that can, at times, impact each other and must be measured carefully.” These conditions include the most common maladies seen by the center’s physicians – memory disorders, hypertension and urinary incontinence – as well as mobility issues, falls, frailty, and excessive use of medications.
“Co-morbidity and fragility, functionally or mentally, are very much at the core of what geriatrics is all about,” he adds. “We also know there will never be enough geriatricians to take care of the growing number of older patients. There are not that many of us nationwide, a fact that drives a big part of the center’s mission to do research and subsequently educate other [non-geriatric] providers on how to take care of older patients.”
The human population has doubled over the past 50 years, in part because we’re living longer. So it has become crucial that the center’s physicians work more and more with colleagues in other disciplines to help with case co-management and to coordinate care of older adults in areas such as orthopedics, cardiology, cancer, dementia and memory disorders.
“As the population ages, there’s more need for well-trained physicians to manage and treat the primary care conditions facing the geriatric population 65 years and older – primarily for memory loss and dementia evaluation, diagnosis and long-term care, and support to the patients, their caregivers and families” says Yazeed Maghaydah, M.D., FACP, an assistant professor of medicine and board-certified internist and geriatrician.
Are we really living longer?
“Life expectancies for people over 65 are expanding by approximately three months per year, and the age group 85 years and older is the fastest growing population in the country – even more than newborns,” says Dr. Kuchel.
As life expectancies continue to rise, many of us will spend more years as older adults than past generations did. That being the case, our quality of life remains the most important part of growing older.
“Years ago, we used to say, ‘If you want to age well, you need to pick your parents carefully,’ ” says Dr. Kuchel. “That’s not quite true. Genetics only play 20% to 30% in the aging process – and that’s the good news – but what actually plays a much bigger role is one’s lifestyle and environment.”
Lavern A. Wright, M.D., is an associate professor of medicine and a board-certified physician in geriatric medicine. In addition to treating UConn Health’s clinic patients, she sees patients in their home environment, such as at Seabury skilled nursing facility in Bloomfield.
“For more than half my patients, I am their primary care provider (PCP). They have common conditions such as high blood pressure, diabetes, cardiac, and memory issues. But I also have a few older patients who have aged successfully and have none of the more common maladies,” says Dr. Wright.
She says that while urinary incontinence is a common health condition in older patients, they are frequently embarrassed to discuss the topic, and the condition has far-reaching social stigma.
“With incontinence comes a reluctance to go out because patients are afraid of wetting themselves,” says Dr. Wright. “You can have social isolation and mood- related issues associated with incontinence. Those with incontinence issues sometimes become institutionalized because it’s difficult to deal with this issue at home.”
The field of geriatrics is the exception to the commonly held “rule” that a physician is either a PCP or a specialist.
“A big part of what we do, in addition to primary care, is consultative care,” says Dr. Coll. “Those of us in medicine sometimes think that a doctor is either a specialist or one who provides primary care. In geriatrics, we have to do both in order to do geriatrics well.”
He says with the exception of pediatricians or neonatologists, every physician who provides health care for adults takes care of some older patients. The patients who really benefit from seeing a geriatrician are “those who struggle with more complex issues.”
Dr. Maghaydah says there are two major ways a patient comes to see a member of his team. In many instances, patients themselves decide they need coaching and guidance through a healthy and successful aging journey, or they may have numerous complicated issues and they and/or family want their care transferred to a geriatric specialist. Or, the patient’s physician and/or family may seek the consultative services of a physician at the Center on Aging or its Memory Disorders Clinic, where a multidisciplinary team will provide an opinion and memory disorders focused management. In the latter scenario, the patient may remain with his or her PCP as that physician and UConn Health work in tandem.
“We’re available to do both – primary and consultative care – but we’re certainly not out to take patients away from their PCPs, particularly when the patient is happy and everything is going well,” says Dr. Kuchel, adding, “our role is to add life to years rather than years to life.”
The Center on Aging’s active research program is multifaceted, focusing on mobility, cognition and behavior, the ability to fend off infection, and voiding and incontinence, thereby helping people to live independently. Research ranges from laboratory work to clinical trials involving the community and large patient populations – such as people in long-term care facilities – all designed to help people age better. For instance, the Center on Aging is currently seeking participants for a hip fracture recovery study.
Each physician agrees there has not been as much progress as they would like surrounding memory issues. Dr. Kuchel says science has “cured Alzheimer’s disease in mice about 300 times now, but getting this cure from mouse models to people is extremely difficult, and we don’t fully understand why.”
“On the basic science level, a lot of work has been and is being done, but unfortunately nothing has materialized, in terms of clinical options,” says Dr. Coll, explaining that Alzheimer’s tends to take a toll on caregivers. “In some cases, the family becomes our patient.”
Are there any breakthroughs in areas involving aging?
“There are a lot,” says Dr. Coll. “In the past, doctors may have traditionally treated patients for diabetes or high blood pressure, and not necessarily thought of the whole person – where they live and work, who they interact with, or what kind of care they have. We’ve done a lot to improve that.”
James Battaglio is a writer living in Glastonbury.
Photography by Connecticut Headshots





More Stories
Over 50, Underestimated: The Grandfluencers Redefining Age on Social Media
Building Resilient Businesses: Strategies for Success
Summer Means Convertibles